We need to prevent people
from becoming patients in the first place
from becoming patients in the first place
By Chris Van Hoof
With the growing pressure on healthcare systems around the world,
the focus today has shifted from treating patients to preventing them from
becoming sick in the first place. Indeed, this has become an important
challenge for any smart healthcare effort.
the focus today has shifted from treating patients to preventing them from
becoming sick in the first place. Indeed, this has become an important
challenge for any smart healthcare effort.
Away from diagnostics and therapy, the emphasis has moved towards
disease prevention and disease interception. While disease prevention mainly
focuses on stimulating (healthy) behavior, disease interception implies
capturing a disease before the first symptoms occur.
disease prevention and disease interception. While disease prevention mainly
focuses on stimulating (healthy) behavior, disease interception implies
capturing a disease before the first symptoms occur.
Both prevention and disease interception require personal digital
phenotyping – the use of digital and wearable technology to track health
parameters and behavior over an extended period of time, so as to identify risk
factors and triggers. To turn this vision into reality, technology innovation
is key.
phenotyping – the use of digital and wearable technology to track health
parameters and behavior over an extended period of time, so as to identify risk
factors and triggers. To turn this vision into reality, technology innovation
is key.
At imec, wearable health R&D has traditionally focused on
developing highly-comfortable, medical-grade wireless solutions for the
diagnosis and management of cardiovascular, neurological and cardiopulmonary
disorders.
developing highly-comfortable, medical-grade wireless solutions for the
diagnosis and management of cardiovascular, neurological and cardiopulmonary
disorders.
Our most recent wireless chest patch in 2017 combines ECG,
respiration rate, respiration depth and actimetry. Due to its compact size and
design, it significantly increases patients’ comfort and can be worn day or
night to screen or diagnose. We are currently running clinical investigational
studies to explore its potential use for patients with congestive heart failure
and chronic kidney disorder.
respiration rate, respiration depth and actimetry. Due to its compact size and
design, it significantly increases patients’ comfort and can be worn day or
night to screen or diagnose. We are currently running clinical investigational
studies to explore its potential use for patients with congestive heart failure
and chronic kidney disorder.
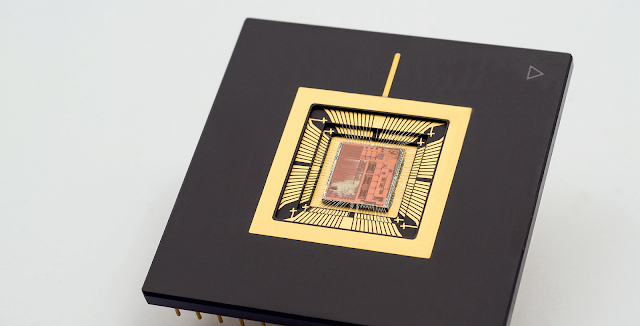
In 2017, we also completed a next generation of our MUSEIC chip, a
low-power multi-(bio)sensor system-on-chip.
It combines a wide range of on-chip electrophysiological sensor readouts
with sensor fusion, powerful (yet ultra-low-power) signal processing, memory,
power management, connectivity, and is at the same time equipped with built-in
security and encryption.
low-power multi-(bio)sensor system-on-chip.
It combines a wide range of on-chip electrophysiological sensor readouts
with sensor fusion, powerful (yet ultra-low-power) signal processing, memory,
power management, connectivity, and is at the same time equipped with built-in
security and encryption.
This platform can be used for very diverse diagnostic applications and
can also feature in smart watches and fitness trackers for wellness assessment.
With such a complex system-on-chip, we can reduce the complexity at the system
and application level.
can also feature in smart watches and fitness trackers for wellness assessment.
With such a complex system-on-chip, we can reduce the complexity at the system
and application level.
The new-generation MUSEIC chip could, for instance, be used to
create a disposable single-use diagnostic smart Band-Aid that people could just
buy at the pharmacy for prescribed diagnostic applications. This could
significantly enhance chronic patients’ comfort and convenience. The expected
cost reduction can also help to bring much needed chronic disease tools to
developing countries.
create a disposable single-use diagnostic smart Band-Aid that people could just
buy at the pharmacy for prescribed diagnostic applications. This could
significantly enhance chronic patients’ comfort and convenience. The expected
cost reduction can also help to bring much needed chronic disease tools to
developing countries.
Digital coaching for a
healthy life
healthy life
Providing accurate diagnosis and efficient treatment tools addresses
an important need, but it would be even better if we could prevent people from
becoming sick in the first place. That is why, in 2017, and after several years
of preparation, we have set up the imec.ichange program, our first step towards
a ‘world without disease’.
an important need, but it would be even better if we could prevent people from
becoming sick in the first place. That is why, in 2017, and after several years
of preparation, we have set up the imec.ichange program, our first step towards
a ‘world without disease’.
According to the WHO, unhealthy behavior and lifestyle are at the
root of nearly 80 per cent of chronic diseases, which in turn are responsible
for 60 per cent of all deaths. Consequently, 70 to 85 per cent of the
healthcare budgets of OECD countries are spent treating chronic patients. This
implies that true prevention has a tremendous potential to save lives and curb
healthcare costs.
root of nearly 80 per cent of chronic diseases, which in turn are responsible
for 60 per cent of all deaths. Consequently, 70 to 85 per cent of the
healthcare budgets of OECD countries are spent treating chronic patients. This
implies that true prevention has a tremendous potential to save lives and curb
healthcare costs.
Digital phenotyping is one of the tools that we can use to prevent
chronic disease. There are already a myriad of fitness trackers and sports
watches that aim to motivate us to make healthier choices and try to make us
fit, but their success rate is unclear: between thirty to fifty percent of
users discard them after 6 months.
chronic disease. There are already a myriad of fitness trackers and sports
watches that aim to motivate us to make healthier choices and try to make us
fit, but their success rate is unclear: between thirty to fifty percent of
users discard them after 6 months.
One of the main reasons is that good intentions are short-lived if
you only focus on maintaining motivation through simple metrics (steps, floors,
heart rate) and generic advice. To achieve a lasting behavior change, we need
to go beyond motivation and focus on people’s personal ability to change by
providing personal triggers.
you only focus on maintaining motivation through simple metrics (steps, floors,
heart rate) and generic advice. To achieve a lasting behavior change, we need
to go beyond motivation and focus on people’s personal ability to change by
providing personal triggers.
This can be accomplished by accurately, unobtrusively and securely
tracking a wider range of physiological parameters and by gathering contextual
information on our behavior, habits, schedule, location and activity.
tracking a wider range of physiological parameters and by gathering contextual
information on our behavior, habits, schedule, location and activity.
Combining detailed physiological data and detailed contextual data
makes it possible to create an individual digital phenotype. This digital
phenotype can then be used to give highly-personalised feedback and suggestions
when you are open to act on them.
makes it possible to create an individual digital phenotype. This digital
phenotype can then be used to give highly-personalised feedback and suggestions
when you are open to act on them.
It urges you to eat healthy just when you are about to walk past the
salad bar towards the fries. It nudges you to take a break after a particularly
stressful meeting or suggests a light snack just when your stress levels
indicate that you are craving that cigarette.
salad bar towards the fries. It nudges you to take a break after a particularly
stressful meeting or suggests a light snack just when your stress levels
indicate that you are craving that cigarette.
Compared to the generic advice now provided by wearables, this kind
of personal feedback provided at the right time is a true paradigm shift.
of personal feedback provided at the right time is a true paradigm shift.
In 2017, we carried out a large-scale study that lays the foundation
for a personalised digital stress coach, focusing on mental health and
well-being. In this study, we did not only measure physiological stress
signals, but we also evaluated self-reported stress and collected contextual
information (via participants’ smartphones).
for a personalised digital stress coach, focusing on mental health and
well-being. In this study, we did not only measure physiological stress
signals, but we also evaluated self-reported stress and collected contextual
information (via participants’ smartphones).
Using wearable technology makes it possible to detect stress outside
of the lab, in a real-life context. However, it also comes with new challenges.
The data might be incomplete or subject to artifacts and we cannot control any
of the context variables.
of the lab, in a real-life context. However, it also comes with new challenges.
The data might be incomplete or subject to artifacts and we cannot control any
of the context variables.
For example, did someone’s heart rate go up because he was
experiencing stress or did he just run up a flight of stairs? For that reason,
we are now developing objective quality indicators to determine when data is
reliable enough to be included in the analysis. A second step will then be to
develop advanced algorithms to mine these large, partially incomplete and
unbalanced datasets.
experiencing stress or did he just run up a flight of stairs? For that reason,
we are now developing objective quality indicators to determine when data is
reliable enough to be included in the analysis. A second step will then be to
develop advanced algorithms to mine these large, partially incomplete and
unbalanced datasets.
The future of smart
healthcare: disease interception
healthcare: disease interception
The grand challenge in smart health is disease interception. Researchers
are trying to establish the link between a disease and the medical factors that
can predict it before any symptoms show.
are trying to establish the link between a disease and the medical factors that
can predict it before any symptoms show.
Wearable technology and artificial intelligence are two of the
ingredients that are part of the solution. The first and foremost challenge
will be rather mundane and practical, that is, finding participants who are
willing to commit to this study in the (very) long term – most likely years.
ingredients that are part of the solution. The first and foremost challenge
will be rather mundane and practical, that is, finding participants who are
willing to commit to this study in the (very) long term – most likely years.
A second challenge will be deciding which parameters we want to
track, because we will only be able to establish what is relevant in hindsight.
And then we need advanced data analytics to make sense of these vast amounts of
heterogeneous data, blurred by real life’s interferences. This is only one part
of a very complex puzzle though.
track, because we will only be able to establish what is relevant in hindsight.
And then we need advanced data analytics to make sense of these vast amounts of
heterogeneous data, blurred by real life’s interferences. This is only one part
of a very complex puzzle though.
We will need to connect this to other components of the human
phenotype to properly understand the probability and causes of disease, and how
a changing phenotype is related to disease emergence. Interception on
individuals at risk is then expected through either pharmaceutical or
non-pharmaceutical channels.
phenotype to properly understand the probability and causes of disease, and how
a changing phenotype is related to disease emergence. Interception on
individuals at risk is then expected through either pharmaceutical or
non-pharmaceutical channels.
This new direction in smart health research will more than ever
require a multidisciplinary approach. You have to bring together different
stakeholders, including not only technical partners (specialised in hardware or
in data analysis), but also partners with medical expertise (hospitals, doctors
and specialists) as well as coaching experts (psychiatrists, psychologists and
behavioral scientists).
require a multidisciplinary approach. You have to bring together different
stakeholders, including not only technical partners (specialised in hardware or
in data analysis), but also partners with medical expertise (hospitals, doctors
and specialists) as well as coaching experts (psychiatrists, psychologists and
behavioral scientists).
At the end of this road, we should be able to truly quantify what it
means to live a healthy lifestyle and how diseases can be intercepted. We may
not quite have reached this goal by 2030, but we hope to do so in our lifetime,
as it would have an impact beyond our wildest dreams.
means to live a healthy lifestyle and how diseases can be intercepted. We may
not quite have reached this goal by 2030, but we hope to do so in our lifetime,
as it would have an impact beyond our wildest dreams.
Chris Van Hoof is an imec
fellow and the director for Connected Health Solutions at imec. A version of
this article first appeared in the imec magazine.
fellow and the director for Connected Health Solutions at imec. A version of
this article first appeared in the imec magazine.
For the LATEST tech updates,
FOLLOW us on our Twitter
LIKE us on our FaceBook
SUBSCRIBE to us on our YouTube Channel!